Breastfeeding is about far more than giving your baby your milk. It is difficult to put into words how breastfeeding our babies makes us feel, but it is a unique experience that most women who have breastfed look back on with fondness and yearning, regardless of whether the experience wasn’t always straightforward or easy, or if she stopped before she planned to. When a woman is having difficulty with breastfeeding, she often feels she has to justify her choice by listing out all the health benefits for her baby. However, there are so many more benefits for mum which I will discuss in the next section.
In the following sections I will discuss the 5 main benefits of breastfeeding namely: Health Benefits for Mum; Health Benefits for Baby; Neurodevelopmental Benefits; Gut Health/Microbiome; and the Social and Environmental Impact of Breastfeeding.
1)Health Benefits for Mum

As mums, we tend to put our needs last so this time I am making them the 1st benefit of breastfeeding. The following is a list of health benefits for mums:
- The baby’s sucking causes the uterus to contract, which reduces blood loss after delivery.
- Breastfeeding provides more than 98% protection against pregnancy, as long as you are exclusively breastfeeding (incl at night), and there has been no postpartum bleeding after the 56th day. This is called the Belaggio Consensus (Wambach and Spencer, 2021).
- Women who breastfeed exclusively burn 200-500 calories extra a day, and lose more weight on average. However if you are trying to lose weight while breastfeeding there are a few things to keep in mind. See https://kellymom.com/nutrition/mothers-diet/mom-weightloss/ for more details.
- Women who breastfeed are less likely to develop breast and ovarian cancer and diabetes in later life. It is well documented that women with Gestational Diabetes are more likely to develop Type 2 Diabetes in later life. Tarrant et al (2020) found that mothers who had gestational diabetes and who exclusively breastfed had improved postpartum glucose regulation which may reduce the risk of developing Type 2 diabetes in later life.
- Breastfeeding is more economical than formula feeding, although I’m not sold on this idea as a universal truth for all. Between breast pumps, nipple shields, Lactation Consultant visits, tongue tie revisions, and alternative therapy’s, breastfeeding costs can add up quite quickly, but it’s totally worth it in my opinion.
- Less trips to the doctor and less money spent on medications as breastfed babies tend to be healthier.
- Breastfeeding enhances the bond between mother and baby. Breastfeeding changes how we parent our babies. We become more responsive to our babies needs, knowing and feeling that many of these needs are met through our physical, social and emotional connection.
- Breastfeeding is a known protective factor for Postnatal Depression. Hormones (oxytocin and prolactin) released during breastfeeding create nurturing feelings of love and calm in mom.
- Getting up at night to feed is a lot easier and faster when you have milk that is ever-ready and always at the right temperature. Having a supportive partner who will get up and change the baby, and bring him or her to you also helps.
- It is just so handy. When you need to pop out all you need is boobs, baby, nappy and spare change of clothes – those poonami’s always happen the minute you set foot outside your door!!!
- Not having to wash and sterilise or make up bottles is always a bonus. Mums who breastfeed, pump and bottle feed are amazing women with superhero status.
2)The health benefits for baby
Colostrum
- This is the first milk mums make and which can be harvested and stored prior to delivering your baby. Colostrum is a yellowish fluid referred to as “liquid gold” which is rich in proteins. These proteins are full of immunoglobulins, antibodies and live cells that give baby an amazing boost to their immune system. The more breastmilk a baby drinks, the greater the immunity (Wamback and Spencer 2021).
- It is thick and less copious so that baby is not overwhelmed with milk as they learn to coordinate their suck, swallow and breathing reflexes.
- The thick colostrum lines the digestive tract like a coat of honey, which prevents pathogens from getting through, leading to a balanced microbiome and therefore a strong immune system.
- Did you know? Mothers of preterm babies produce even higher levels of protein and fat compared with mothers of term babies, in order to give the preterm baby that additional boost of immunities and fat content. Half of the baby’s body fat accumulates in the last 5 weeks of gestation, therefore mothers of preterm babies produce milk with higher fat content in order to compensate for this (Wambach and Spencer 2021). Amazing!!
Other Health Benefits

- Fat content – Did you know that fat in human milk varies greatly from feed to feed and is directly proportional to how much/often the breast is emptied. A full breast has a lower fat content, but as a breast empties the fat content of the remaining milk increases. Therefore, the more often a baby feeds the higher the fat content. A longer interval between feeds = lower fat content (Wambach and Spencer, 2021).
- Fat content is higher during the day and lower at night. Breastfeeding mama’s who are establishing supply are encouraged to feed at night, but this is because Prolactin levels are higher at night and prolactin affects 24 hour milk production.
- Breastmilk contains everything a baby needs to grow and thrive, except Vit D (in sufficient amounts), which needs to be supplemented here in Ireland, as we don’t get enough sunlight.
- Interestingly, mothers of male babies produce milk that is 25% higher in energy content than mothers of female babies.
- Appetite regulation – Breast milk contains Leptin which helps baby to feed on demand and not ‘over-feed’. Exclusively breastfed babies weigh the same or more as bottle-fed (formula/combi-fed) babies at 3-4mths. However after this time bottle fed babies weigh more on average, as their volume increases over time as they get older. Breastfed babies feed on demand and have Leptin to help them to regulate their appetite. Parents will often observe their babies only taking 5 minute feeds every few hours and worry about whether they are getting enough. But that worry stems from our cultural expectation that a set number of ounces every 3-4 hours is required as the ‘norm’. This is simply not true for the established breastfed baby.
- Breastfeeding promotes the ideal development of babies’ jaw and teeth (Watson Genna, 2017)
- Babies who breastfeed exclusively are at a lower risk for
- SIDS (Sudden Infant Death Syndrome)
- Ear Infections
- Diarrhoea
- Pneumonia
- Diabetes
- Stomach bugs
- Obesity
- Childhood Cancers
- Heart Disease
(Carolina Global Breastfeeding Institute 2020)
3)Neurodevelopmental benefits

This can be a contentious issue but breastfed babies have higher IQ’s than non-breastfed babies. Studies have shown that adolescents who were breastfed had increased total white matter, as well as higher IQ’s with a correlation to length of time breastfeeding (Wambach and Spencer, 2021). This is not to say that all formula fed babies have lower IQ’s. This is definitely not the case. The research supports the theory that ‘on average’ breastfed babies have higher IQ scores. Horta et al (2018) also confirmed that there is a positive correlation between breastfeeding and higher IQ in adulthood, but could not say whether this was due to the effect of human breastmilk or the mother-infant interaction whilst breastfeeding. This brings us nicely to the next section, which I think is simply fascinating.
According to Watson Genna (2017) all the neurons a baby can use form in the baby’s brain by 28 weeks gestation. Not all these neurons will be used. The neurons that aren’t stimulated or ‘fired’ don’t wire. In other words: Use them or lose them!! Stimulation of the baby such, as being held by its parents, kissed, cuddled, and fed causes certain neurons to fire and in turn, hard wire into established pathways. For example, a baby cries when he/she wants to be held. If parents consistently deny this, those neurons don’t hardwire and they die off, thus babies stop seeking this emotional comfort and reassurance.
From term (40 weeks) until the baby is 1 year, these neurons are ‘pruned’, and removed depending on their physical, social and emotional experiences, and by the end of that first year the baby’s brain is hard-wired.

When the baby is in utero, conditions for optimal neural pathways to be laid down are ideal and pretty consistent. However once the baby is born, he or she is completely dependent on his or her parents, and their ability and desire to provide that physical, social and emotional stimulation. Delivery and skin-to-skin are baby’s first stimuli. Self-attachment to the breast is the next predictable, specific step baby takes, usually within 1 hour of delivery, if the birth is un-medicated. After this first feed, baby normally falls into a deep sleep for 3-6 hours while skin-to-skin. This is extremely important in achieving “the wiring that came from the firing” (Watson Genna, 2017, pp 55). This process continues for virtually all aspects of newborn life including thermoregulation, bonding, and cardio-respiratory balance. For anyone interested in reading more about this and much more Catherine Watson Genna’s “Supporting Sucking Skills for Breastfeeding Infants” is an excellent book, brilliantly written and endlessly fascinating for a nerd like me.
4)Gut Health/Microbiome

The ‘microbiome’ refers to a population of microorganisms that exist in the human body, and upon whom we humans are dependent on to keep us alive and healthy, including fungi, parasites and bacteria (Wimberly Groer et al. 2020). If the balance of these microorganisms is compromised, as often occurs with yeast resulting in thrush, we can have health repercussions.
Breastfeeding provides the most consistent early source of probiotic bacteria, which includes staphylococcus (mums skin bacteria), infant saliva bacteria and bacteria produced in the milk glands (Wimberly Groer et al. 2020). Breast milk delivers 800,000 bacteria daily directly to the baby’s mouth and GI tract. Babies who are formula fed will receive environmental pathogens and will have higher amounts of gut bacteria, but they are far less diverse and are missing the highly specialised human milk microbiome (Oki et al 2018 cited in Wimberly Groer et al 2020).

Factors that affect the microbiome:
- Mode of birth
- Breastfeeding stage
- Gestational age
- Medicines and antibiotics
- Genetics
- Maternal diet and lifestyle
- Geographic location
- Overall health status
(Wambach and Spencer, 2021)
So how does the microbiome affect infant health?
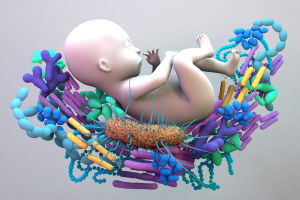
When a newborn drinks colostrum, it coats the gut wall in a thick honey like substance that is packed with probiotics and good bacteria, and proteins that optimize immunity. These proteins are full of immunoglobulins, antibodies and live cells that give baby an amazing boost to their immune system. The more breastmilk a baby drinks, the greater the immunity (Wamback and Spencer 2021).
- The microbiome has been implicated in allergy and asthma conditions. Different microbes dwell in specific areas, meaning that there are various specific microbiomes present in the body including the gut, lungs, and skin. The theory is that these microbiomes are connected and this “microbial dysbiosis in the gut and lung is increasingly being associated with the incidence and severity of asthma” (Sokolowska et al 2018, p.1).
- It is linked to infant overweight and obesity.
- Certain strains may ameliorate the symptoms of rotavirus.
- There are some who consider the rise in autoimmune conditions as linked to the formula feeding culture that has been predominant since the 1950’s and 1960’s, but there is no concrete evidence to support this theory, to my knowledge.
5)The Social and Environmental Impact of Breastfeeding

The Environmental Impact
This benefit is discussed a lot less than the others, and in terms of immediate importance to the mum and baby dyad, we can understand why. However breastfeeding significantly reduces the human environmental impact on our planet.
- Breastmilk is a naturally renewable resource that costs very little extra to produce, and requires no advertising, manufacturing, shipping or disposal, thereby reducing fuel and electricity consumption.
- Infant formulas require mass production on an industrial scale, with plastic and other waste affecting our land and waterways.
- Infant formula is made from cow’s milk. Livestock is responsible for 20% of greenhouse emissions, therefore infant formula is one of the most emissions-intensive foods to be produced (Gulbransen 2020), particularly in Ireland where infant formula remains a fundamental element of the Irish dairy export industry (which was worth over €900m in 2019, and from which China accounts for 36pc of total exports) (Moran 2020).
- Cows feed on grass in large fields or pastures, some of which was previously forested land, which has been cleared for cattle grazing. Forests and trees absorb and store much of the carbon dioxide that would otherwise be contributing to climate change Therefore, when forests are cleared to make way for cattle grazing land, our environment takes a double hit (Smith 2019).
- Ireland makes 10% of the formula fed to babies around the world, which if you think about the size of our little country, this is a significant fact. Another significant fact is that bottles of formula are still being given out freely in Irish Maternity Hospitals, and if a mother chooses to top-up her baby in the hospital, the brand she chooses is usually the brand she stays with on discharge. These formula companies supply this formula for free to Irish hospitals, therefore it is a lucrative form of charity for formula companies. This may go some way in explaining why only 60% of Irish women leave hospital breastfeeding compared with 90% in Australia and 81% in Britain (Nī Chonchūir 2020). However there are other contributing factors also, which include poor antenatal education, lack of IBCLC’s as staff in Irish Maternity Hospitals, the medicalising of birthing and feeding in Ireland, as well as our lost generational support for breastfeeding in Ireland.
The Social Impact
- Child-spacing- Breastfeeding provides more than 98% protection against pregnancy, as long as you are exclusively breastfeeding (including at night), and there has been no postpartum bleeding after the 56th day. This is called the Belaggio Consensus (Wambach and Spencer, 2021). While child spacing is not such a concern in the developed world, in poorer countries it helps parents to focus all the nutritional benefits on one child at a time, therefore improving outcomes.
- Improved vaccine effectiveness – breastfed babies appear to have better serum responses to vaccines that are administered orally (such as the Rotavirus Vaccine).
- Improved Public Health – Breastfed babies and mothers tend to be healthier (See Health Benefits for Babies and Mums Sections), with fewer acute and chronic illnesses experienced. This benefits the state’s pockets and frees up valuable Hospital resources to other people. Breastfed babies have 15% fewer GP consultations in the first 6 months of life than formula fed babies, and they are 5 times less likely to be hospitalised with Gastroenteritis (La Leche League 2020).
- Decreased Employee Absenteeism- Mothers who breastfeed have fewer sick days as their infants tend to be very healthy. Studies also show that mothers and other employees tend to feel more positive about companies that support them in continuing to breastfeed and this leads to increased worker retention (Wiessinger et al 2017, Wambach and Spencer 2021). See https://latchingon.ie/postnatal/breastfeeding-and-returning-to-work/ for more information on Breastfeeding and Returning to Work in Ireland.

Conclusion
The discussion around breastfeeding is about far more than simply breastmilk. It is about how we view and treat our bodies, our relationships, our communities and our world. Formula will certainly always be valuable and have a place in modern societies, but the narrative should never be Formula vs. Breast. There is no competition. From every perspective, the choice to breastfeed your baby is the best choice, but that does not mean that formula is unimportant. It is very important, in that for the majority of babies born in Ireland since the 1950’s and 1960’s, formula milk has nourished and grown most of these babies to healthy adults. Formula feeding continues to be the predominant method of feeding Irish babies today, and there are many reasons for this.
We must continue to educate ourselves and others around us on the value of breastfeeding, without derogation for others’ choices. We, who work in lactation and breastfeeding must endeavour to generate significantly more roles in Lactation within hospitals and communities and businesses, including breastfeeding counsellors, Lactation Consultants and peer supporters. There needs to be greater collaboration and information sharing between health care providers, alternative therapists, pharmacists, volunteers and parents. But it needs to begin within communities, not from centralised centres of excellence. The GAA is a grass-roots organisation whose mission is: “a community based volunteer organisation promoting Gaelic Games, culture and lifelong participation” (GAA 2020). The foundations that the GAA are built on are community involvement and lifelong participation. There is much we can learn from how the GAA has continued to bring villages and communities together to achieve a common goal, and I believe that with enough time, enthusiasm, participation, energy and resources, there is no reason why breastfeeding rates in Ireland cannot match or exceed those of our European counterparts.

References
Carolina Global Breastfeeding Institute (2020) Ready, Set, Baby: A guide to welcoming your new family member (Online). https://sph.unc.edu/files/2017/08/CGBI_RSB-V3-Booklet-2018_SW.pdf (Accessed on 10/12/2020).
Gaelic Games Association (2020) GAA Mission, Vision, and Values (Online). https://www.gaa.ie/the-gaa/administration/ [Accessed 02/01/2021)
Gulbransen K. (2020) Pros of Breastfeeding for Baby, You and The Planet (Online) https://www.greenchildmagazine.com/breastfeeding-good-for-you-baby-and-planet/ [Accessed on 02/01/2021].
Horta B.L. Hartwig F.P. Victoria C.G. (2018) “Breastfeeding and intelligence in adulthood: due to genetic counselling?” The Lancet, vol. 6, pp 1276-1277, viewed on 10th December 2020, https://www.thelancet.com/action/showPdf?pii=S2214-109X%2818%2930371-1.
La Leche League (2020). Breastfeeding and the Environment (Online). https://www.laleche.org.uk/breastmilk-and-the-environment/ [Accessed 02/01/2021).
Moran C. (2020) Tougher rules on infant formula advertising to protect breastfeeding (Online). https://www.independent.ie/business/farming/agri-business/tougher-rules-on-infant-formula-advertising-to-protect-breastfeeding-39142386.html [Accessed on 02/01/2021].
Smith J.P. (2019). “A Commentary on the carbon footprint of milk formula: harms to planetary health and policy implications” (Online) International Breastfeeding Journal 14 (49), p.1. [Accessed on 15th January 2021].
Sokolowska, M., Frei, R., Lunjani, N. et al. Microbiome and asthma (Online). asthma res and pract 4, 1 (2018). https://doi.org/10.1186/s40733-017-0037-y [Accessed on 02/01/2021].
Tarrant, M. Chooniedass, R. Sze Lok Fan, H. Del Buopne, K. Masina, S. (2020) “Breastfeeding and Postpartum Glucose Regulation Among Women with Prior Gestational Diabetes: A Systematic Review”, Journal of Human Lactation, vol.36, no.4, pp 723-738, viewed on 10th December 2020, https://journals.sagepub.com/doi/pdf/10.1177/0890334420950259.
Wambach K. and Spencer B. (2021) Breastfeeding and Human Lactation (6th Ed). Jones and Bartlett Learning: Burlington, Massachusetts.
Watson Genna, C (2017) 3rd Ed, Supporting Sucking Skills in Breastfeeding Infants, Jones and Bartlett, Burlington, MA.
Wimberly Groer, M. Hope Morgan, K. Louis-Jacques, A. Miller, E.M. (2020) “A Scoping Review of Research on the Human Milk Microbiome”, Journal of Human Lactation, vol.36, no. 4, pp 628-643, viewed on 10th December 2020, https://journals.sagepub.com/doi/pdf/10.1177/0890334420942768.

